Interactive keyword/Map Sales Tool for Location based physical sales - need better name
Remedy
INDUSTRY
HEALTHCARE
Type
SAAS

HEALTHCARE
SAAS


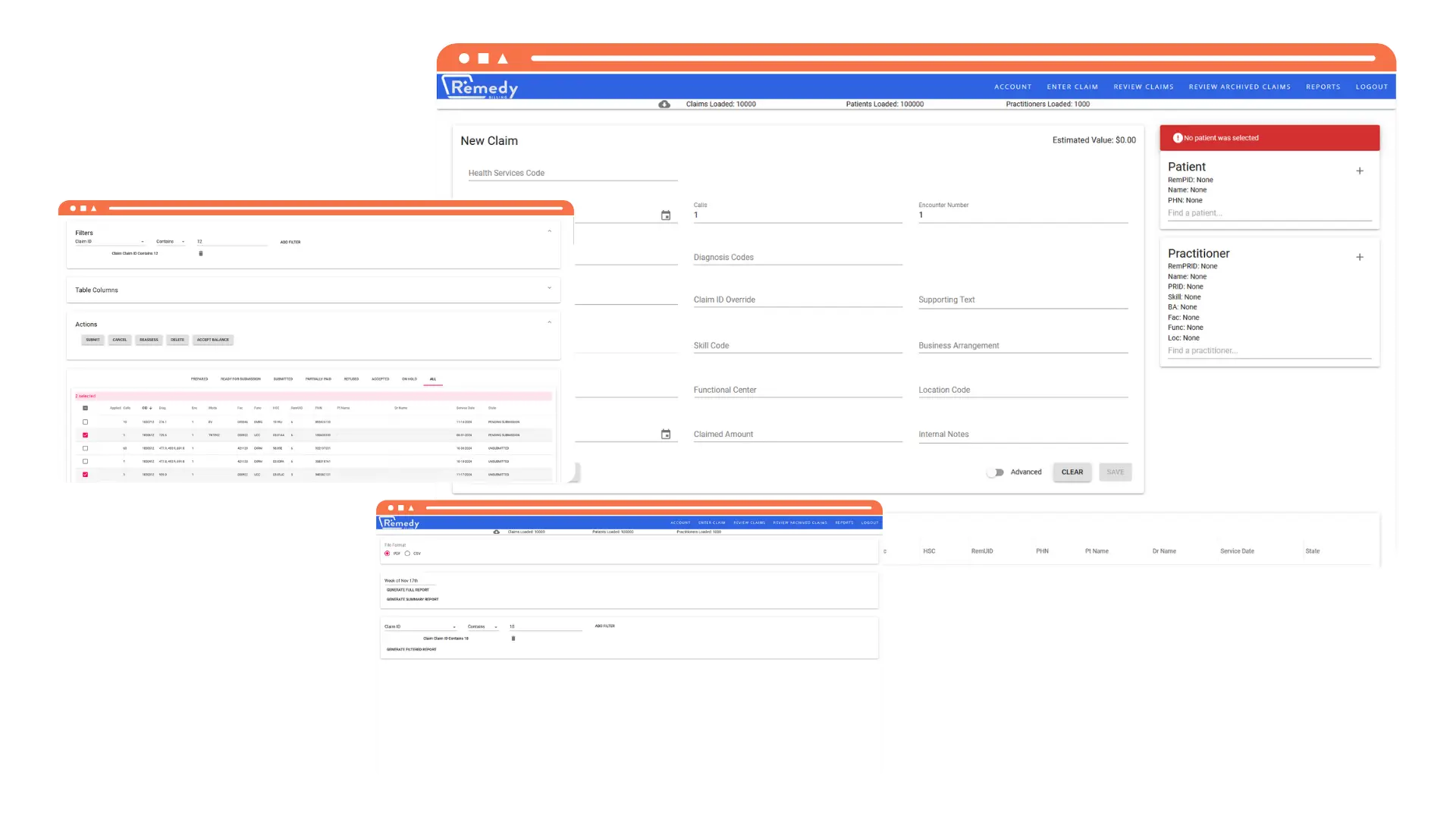
Implemented a system to monitor an SFTP server for new claim files, ensuring timely processing.
Streamlined the process of extracting, validating, and transforming claim data, reducing manual effort and errors.
Ensured data integrity and traceability through comprehensive validation checks and logging mechanisms.
Improved security features to protect sensitive medical and billing information.
Enabled the client to upgrade to the new integration without any disruption to their services.







Automated the claims processing workflow, significantly reducing the time and effort required for manual processing.
Ensured compliance with the latest standards set by AHS and EPIC, keeping the client’s system up-to-date.
Enhanced the security of the claims processing system, protecting sensitive data and maintaining patient confidentiality.
Facilitated a smooth transition to the new integration, allowing the client to maintain uninterrupted service.